How Many Layers Of Skin Does A Tattoo Go Through
Tattoo Ink - Where Does Information technology All Go?
Disclaimer: All images here are rough representations. Please read the text, not just the caption, for a full caption. Likewise, the data presented here is in no style guaranteed to be consummate, yet I have tried to piece together as much of the puzzle as possible. Experience free to contact me if errors or omissions are institute.
Contents:
Introduction
Jargon - feel free to skip this department, but information technology may be useful to refer to while reading the text
The Skin
- Epidermis
- Dermis
Tattoo Ink Placement
Stages of Ink Dispersal
- Then why does the tattoo fade over time?
- What nigh the sun?
Introduction:
Tattoo ink dispersal in the pare has not been thoroughly studied despite the long history of tattooing. The following is any I accept managed to piece together from journal articles and textbooks. For those of you who would like to read the original science jargon, or to read nigh unlike ink particle sizes (depends on the colour) cheque out these links:
Tattoo Ink Removal - Covers the Location of Tattoo Ink and Ink Particle Sizes
A Lecture Well-nigh Skin - Covers Cellular Particular
Jargon:
These are some definitions that may be useful.
Extracellular - exterior of the cell
Intracellular - within the cell
Phagocytosis - think of information technology as the jail cell swallowing an particular east.g. a particle of tattoo ink
Phagocytic - cells that are capable of phagocytosis; some cells can become phagocytic during an inflammatory response (e.g. keratinocytes), whereas others are phagocytic all the time (e.g. many immune cells).
Dendritic Cell - an allowed cell blazon that continually samples its environs for changes, and will migrate to lymph nodes to trigger an immune response if necessary.
Mast Cell - an allowed cell that plays a crucial role in allergic reactions and is present in connective tissue.
Extracellular matrix - a generic name for the scaffold of proteins (both structural and "gum" types) that cells adhere to and are supported by. Major components include basement membrane (one type of collagen network), rubberband fibers, structural glycoproteins (eastward.grand. fibronectin), proteoglycans("glue") and collagen.
Fibrocyte - a cell type that makes up about of the cells in connective tissue. They secrete collagen as well as other proteins that make up the extracellular matrix when activated. They are not commonly phagocytic, merely become so when inflammation occurs.
Fibroblast - a fibrocyte that is actively secreting proteins (an active fibrocyte).
Granulation tissue - tissue that fills in gaps formed from debris or necrotic tissue removal. It consists of newly formed small blood vessels embedded in a loose structure of fibroblasts and immune cells. As the tissue matures, immune cells decrease in number, fibroblasts form collagen networks and blood flow resumes to the area.
The Pare
The skin is made up an outermost layer named the epidermis, followed by the dermis and the hypodermis.
· Epidermis : composed mostly of keratinocytes, cells that contain keratin, the poly peptide that gives skin its toughness (not to exist dislocated with collagen which gives pare its resiliency).
· Dermis : a network of elastic dense connective tissue containing collagen likewise as sweat glands, hair follicles, sebaceous ("oil") glands, nervus endings and blood vessels.
· Hypodermis : loose connective tissue containing by and large adipose (fat) tissue.
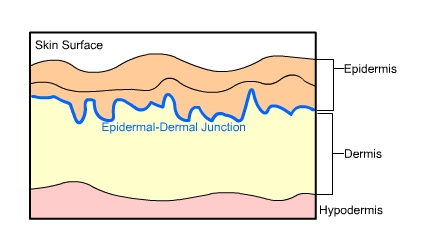
Fig.one The 3 Layers of the Skin
Epidermis
The epidermis is separated from the dermis past a basement membrane (an extracellular network of collagen fibers that serves as a support framework for cells) that strengthens the interface between the epidermis and dermis to preclude tearing from excessive stretching.
There are five layers of the epidermis, where the surface layers are regenerated from stem cells in the deepest layer that differentiate equally they motion outwards:
· Stratum basale (deepest)
· Stratum spinosum
· Stratum granulosum
· Stratum lucidum
· Stratum corneum (surface)
Briefly, the stratum basale contains keratinocyte stalk cells ("basal cells") that are continually dividing to create new cells. These cells differentiate, or in other words change, as they migrate through the layers to the surface. The stratum granulosum is the "waterproofing" layer of cells, and cells no longer divide at this level. The outermost surface layer is composed of dead keratinocytes which are substantially cells filled with keratin.
Dermis
The dermis, a connective tissue made upward of collagen and networks of elastic fibers which requite skin its resiliency, is the layer in which tattoo ink is deposited. The dermis (papillary layer) immediately below the epidermis is made of loose connective tissue and contains small blood vessels and nerve endings. The residue of the dermis (reticular layer) is fabricated of dumbo connective tissue and contains blood vessels, hair follicles, sweat glands, lymphatics, fretfulness, and sebaceous glands.
The majority cell type in the dermis is fibrocyte (or fibroblast). These cells secrete the proteins that brand up the connective tissue network. Other cells that are important in relation to tattoo ink are resident immune cells. These include dendritic cells, macrophages, and mast cells.
Tattoo Ink Placement
The tattooing process causes impairment to the epidermis, epidermal-dermal junction, and the papillary layer (topmost layer) of the dermis. These layers appear homogenized (or in other words, like mush) right after the tattooing process. The ink itself is initially dispersed as fine granules in the upper dermis, only aggregate into more concentrated areas at 7-thirteen days.
Like whatever injury, the initial response is to cease haemorrhage, followed by tissue swelling, and the migration of not-resident immune cells into the area. The "automatic response" allowed cells are by and large neutrophils, and macrophages afterwards on. They are phagocytic cells that "swallow" debris to make clean upwards the area and then get out via the lymphatics. This is the extent of an allowed response unless an allergic reaction occurs or an infection sets in. The tissue is so repaired and/or regenerated past fibroblasts. Initially the tissue formed is known as granulation tissue (retrieve fresh scar, pink and soft), which afterwards matures into fibrous tissue (remember old scar).
Stages of Ink Dispersal
Initially ink is taken upwardly by keratinocytes, and phagocytic cells (including fibroblasts, macrophages and mast cells).
At one calendar month the basement membrane of the epidermis (epidermal-dermal junction) is reforming and the basal cells contain ink. In the dermis, ink containing phagocytic cells are concentrated along the epidermal-dermal junction below a layer of granulation tissue that is surrounded by collagen. Ink is notwithstanding being eliminated through the epidermis with ink present in keratinocytes, macrophages and fibroblasts.
At two to 3 months the basement membrane of the epidermis is fully reformed, preventing whatsoever further loss of ink through the epidermis. Ink is now nowadays in dermal fibroblasts. Almost of these ink containing fibroblasts are located beneath a layer of gristly tissue which has replaced the granulation tissue. A network of connective tissue surrounds and effectively traps these fibroblasts. It is assumed that these fibroblasts are the cells that give tattoos their lifespan.
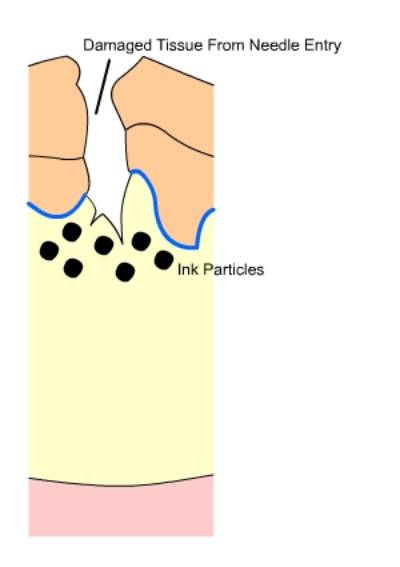
Fig.ii Injured Tissue: Ink is deposited into the upper surface of the dermis upon needle entry.
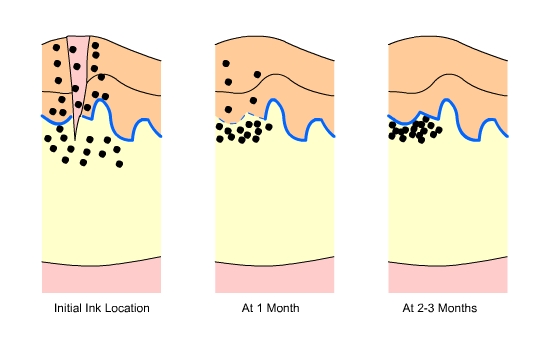
Fig.three Ink Location: soon subsequently the tattoo is received, one calendar month later, and two to three months after. Note the reformation of the epithelial-dermal junction over time and the concentration of ink merely underneath information technology.
So why does the tattoo fade over time?
It is debated whether all the ink particles are in fibroblasts, or if some remain as extracellular aggregations of ink. Also, the lifespan of the ink containing fibroblasts is non known. Presumably, ink particles are moved into the deeper dermis over time due to the action of mobile phagocytic cells (think immune cells), causing the tattoo to look blue, faded and blurry. Examination of older tattoos (e.g. twoscore years) show that the ink is in the deep dermis, and as well found in local lymph nodes. Since some types of phagocytic immune cells migrate to lymph nodes to "present their appurtenances", the discovery of ink in lymph nodes is consistent with the theory of phagocytic cells beingness the cause of ink movement.
What about the sunday?
Sun exposure equals dominicus damage, whether y'all realize it or not. Langerhans cells, a type of dendritic prison cell, are present throughout the epidermis, but mostly located in the stratum spinosum. During sun exposure, many Langerhans cells will undergo apoptosis (a type of cell death where the cell breaks apart into many pocket-size fragments) while others migrate into the dermis and a pocket-sized inflammatory reaction occurs. The inflammatory reaction is not restricted to the epidermis, but also involves the dermis. Such a reaction causes the recruitment of more phagocytic immune cells to the surface area.
With the presence of larger than normal amounts of migrating phagocytic cells, the chances of ink movement increases, thus accelerating the fading of the tattoo.
Compiled: January xiii 2003
been edited. We can non guarantee that the experience is accurate, true,
or contains valid or even safe communication. We strongly urge y'all to utilise BME and
other resources to educate yourself so you can make rubber informed decisions.
Source: https://archives.evergreen.edu/webpages/curricular/1999-2000/humanbio/TattooInk.htm
Posted by: spauldingletly1953.blogspot.com


0 Response to "How Many Layers Of Skin Does A Tattoo Go Through"
Post a Comment